Posterior Tibial Tendon Dysfunction and Acquired Flat Foot Deformity
What is posterior tibial tendon dysfunction and acquired flat foot deformity?
Posterior tibial tendon dysfunction is a common condition resulting from trauma or overuse injury to the tendon of the tibilais posterior muscle in the lower leg. In its early stages it may present as pain +/- swelling on the inside (medial aspect) of the ankle in association with weight bearing activities such as walking and running. As it progresses the medial longitudinal arch of the foot may begin to flatten, resulting in an acquired flat foot deformity. An acquired flat foot deformity occurs because the structural integrity of the arch is compromised and can no longer fully resist the loads imposed upon it.In the absence of trauma, the development of a flat foot deformity typically occurs gradually and in its early stages mainly involves soft tissue structures. At this point the deformity is flexible, however, as the condition progresses arthritic changes can develop, ultimately resulting in a rigid deformity. Along the way tolerance of weight-bearing activities diminishes with implications for the performance of activities of daily living, sporting/recreational pursuits and social endeavours.
The condition most commonly affects females over 40 years of age, overweight individuals, those with pre-existing flat feet and those with certain medical conditions (e.g. connective tissue disorders, diabetes and rheumatoid arthritis). Active younger people may also develop the condition secondary to overuse, lower limb weakness and/or sub-optimal biomechanics.
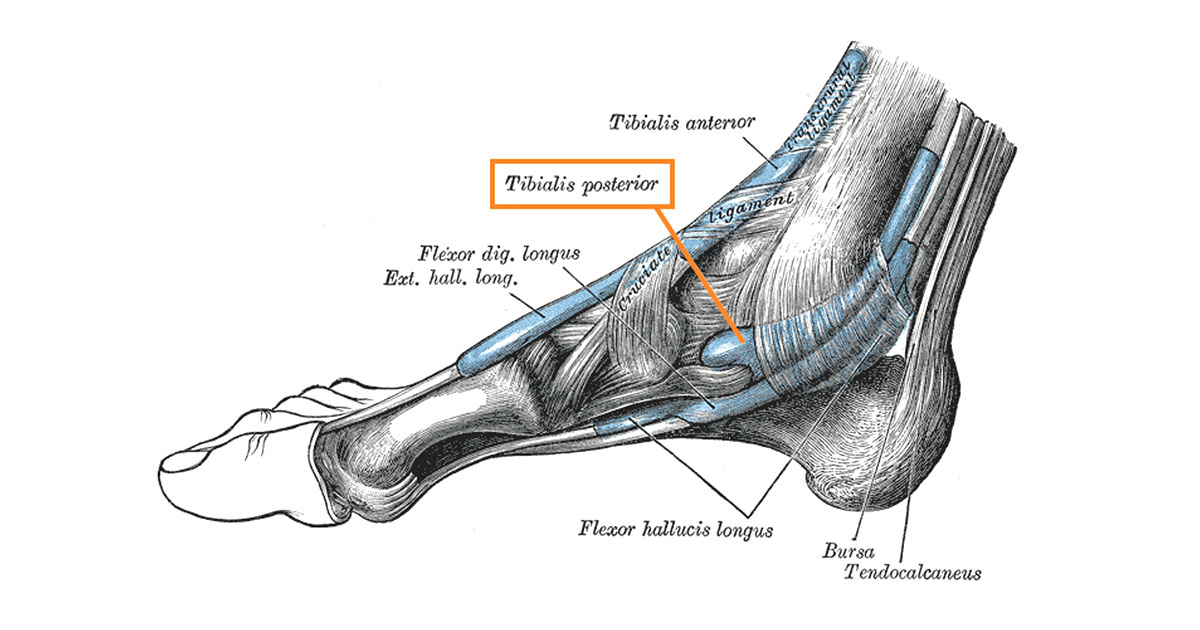
Basic anatomy
The tibialis posterior is a muscle of the lower leg situated deep to the calf muscles and attaching mainly to the back of the tibia (shin bone). Its tendon passes behind the inner (medial) aspect of the ankle joint and carries on to attach to a number of bones in the medial mid-foot region (figure 1). It acts to help you raise up on your toes and plays in important role in actively supporting the structure of the medial arch and stabilising the ankle. Other structures providing support for the arch include musculature within the foot, the plantar fascia and a number of ligaments under the mid-foot. Of the latter, the calcaneonavicular (spring) ligament is of particular importance and is frequently compromised as a consequence of posterior tibial dysfunction.Signs and symptoms of tibialis posterior dysfunction and acquired flat foot deformity?
Pain +/- swelling is usually experienced along the course of the tibialis posterior tendon behind the bone of the medial ankle (medial malleolus of the tibia) and towards its attachment in the mid-foot region. In its early stages, pain is typically experienced at the commencement of weight-bearing activity and then diminishes as you move around (warm-up effect). Increased pain/stiffness may then be experienced later in the day after a period of inactivity, or the next morning after getting out of bed. As the condition progresses this warm-up effect often becomes less pronounced to the point that pain may just progressively worsen with activity. More significant pain, swelling and stiffness may also be experienced after activity and for longer durations. Discomfort and pain may also begin to be experienced in other regions of the foot such as under the arch and heel, as well as in the ankle. Alterations in movement patterns and reduced physical conditioning may also result in other parts of the lower body becoming symptomatic (e.g. pain in the hip, knee and/or low back).Management
With early diagnosis and appropriate management, it may be possible to slow or halt progression of the condition by conservative means. This often includes the use of advice/education about the condition and self-management strategies, an individualised program of strengthening and stretching to address deficits identified during your assessment, footwear advice and the use of a supportive foot orthotic or ankle/foot orthosis. In some cases a period of immobilisation and reduced weight bearing of the foot/ankle may be indicated to allow injured structures time to heal.In more advanced cases conservative management may not be sufficient to adequately address pain and loss of lower limb function, in which case the opinion of a foot and ankle specialist may be required. The specialist can then make the determination as to whether to continue with conservative care or proceed to surgical intervention in order to address underlying structural deformity and/or tendon insufficiency. If surgery is undertaken then a progressive rehabilitation program supervised by a physiotherapist is advised.
Given that increased body weight is a risk factor for developing the condition, weight loss strategies are often beneficial for overweight/obese individuals.
Role of physiotherapists in the management of posterior tibial dysfunction
Physiotherapists are frequently involved in the assessment, conservative management and post-surgical rehabilitation of posterior tibial dysfunction, along with other practitioners such as podiatrists and medical professionals. At Carina Central Physiotherapy, all our physiotherapists are either Titled Musculoskeletal or Sports and Exercise Physiotherapists, meaning that they have all undertaken post-graduate study and have extensive experience in these fields. We therefore have the skills and knowledge to assess and diagnose this condition, and to implement a high-quality management plan.
REFERENCES
Beeson, P. (2014). Posterior Tibial Tendinopathy: What Are the Risk Factors? Journal of the American Podiatric Medical Association, 104(5), 455-467.
Brukner, P., & Khan, K. (2012). In Clinical Sports Medicine (4th ed). McGraw-Hill Astralia Pty Ltd.
Deland, J. T., de Asla, R. J., Sung, I.-H., Ernberg, L. A., & Potter, H. G. (2005). Posterior Tibial Tendon Insufficiency: Which Ligaments are Involved? Foot & Ankle International, 26, 427. doi:10.1177/107110070502600601
Rabbito, M., Pohl, M., Humble, N., & Ferber, R. (2011). Biomechanical and Clinical Factors Related to Stage I Posterior Tibial Tendon Dysfunction. Journal of Orthopaedic and Sports Physical Therapy, 41(10), 776-784.
Ross, M. H., Smith, M. D., Mellor, R., & Vicenzino, B. (2018). Exercise for posterior tibial tendon dysfunction: a systematic review of randomised clinical trials and clinical guidelines. BMJ Open Sport & Exercise Medicine, 4:e000430. doi:10.1136/bmjsem-2018-000430
